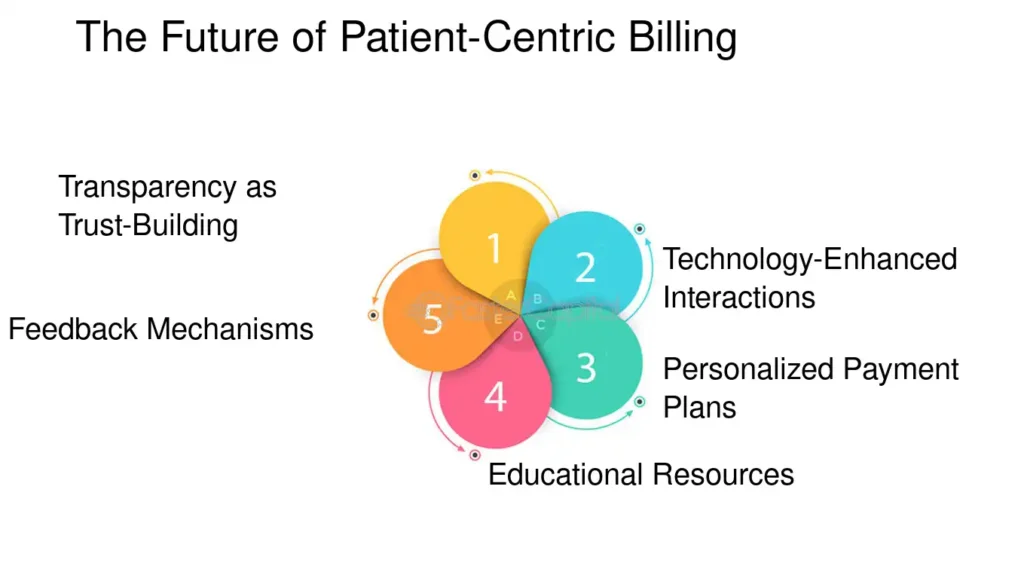
In today’s healthcare landscape, patient satisfaction goes far beyond quality clinical care. Financial interactions—including billing practices—play a crucial role in shaping a patient’s overall experience. Patient-centric billing is all about making the billing process transparent, understandable, and stress-free for patients. By adopting strategies that focus on clarity and customer service, healthcare providers can build trust, improve satisfaction, and even enhance their revenue cycle management.
Understanding Patient-Centric Billing
Traditional billing methods often leave patients confused with lengthy invoices and complicated medical codes. Patient-centric billing reimagines this process by focusing on the needs of the patient. It involves clear communication, easy-to-understand billing statements, and proactive support to address any questions or concerns. This approach ensures that patients are well-informed about their financial responsibilities and can make decisions confidently regarding their healthcare expenses.
Why Transparency Matters
Transparency in billing not only builds trust but also minimizes the risk of billing disputes and delays in payments. When patients clearly understand what they are being charged for, they are more likely to pay on time and feel satisfied with the services they receive. This open communication can also reduce the number of billing inquiries and the administrative burden on your office, allowing your team to focus on delivering quality care.
Key aspects of transparency in billing include:
- Clear Breakdown of Charges: Instead of a long list of codes, provide a simplified breakdown of the services rendered and their associated costs.
- Accurate and Timely Statements: Ensure that invoices are sent promptly and accurately reflect the care provided.
- Accessible Communication Channels: Offer multiple avenues for patients to ask questions or resolve issues—whether through a dedicated billing hotline, email, or online portal.
Enhancing Patient Satisfaction
Patient-centric billing directly impacts satisfaction by making the financial side of healthcare as seamless as possible. When patients have a positive billing experience, it enhances their overall perception of the healthcare provider. Here are some benefits:
- Reduced Confusion and Stress: Simplified billing statements help patients understand their expenses, leading to reduced anxiety over medical bills.
- Improved Patient-Provider Relationship: Transparent billing practices can foster trust and open communication, making patients more likely to stick with your practice.
- Increased Payment Compliance: When patients are informed and satisfied, they’re more likely to pay their bills promptly, which improves the overall financial health of the practice.
Implementing Patient-Centric Billing Practices
Successful patient-centric billing requires a combination of technology, process improvements, and effective communication. Consider these strategies:
- Invest in Modern Billing Software:
- Utilize advanced billing solutions that can generate clear, concise invoices and automate repetitive tasks. This technology can help ensure accuracy while freeing up staff to focus on patient interactions.
- Automated systems can also offer patients online payment options, making it easier for them to settle bills at their convenience.
- Simplify Billing Statements:
- Replace medical jargon and complex codes with plain language explanations that patients can easily understand.
- Include visual aids, such as charts or infographics, to break down charges and illustrate where each cost is coming from.
- Enhance Communication:
- Provide a dedicated billing support team that can quickly address patient inquiries and resolve billing issues.
- Develop clear, accessible resources—both online and in print—that explain the billing process, insurance coverage, and payment options.
- Offer Flexible Payment Options:
- Introduce payment plans or financing options to accommodate patients with varying financial situations.
- Consider partnerships with third-party payment processors that specialize in healthcare to ensure secure and convenient transactions.
- Regularly Review and Update Processes:
- Continuously gather feedback from patients regarding their billing experience.
- Use this feedback to refine processes and implement improvements that make the billing process even more user-friendly.
How InvoQuest Supports Patient-Centric Billing
At InvoQuest, we understand that a patient-friendly billing process is integral to both patient satisfaction and a healthy revenue cycle. Our solutions are designed to automate billing tasks, reduce errors, and provide clear, understandable billing statements. By focusing on patient-centric practices, we help healthcare providers build trust, improve collections, and ultimately enhance the overall patient experience.
For more information on how our billing solutions can transform your practice, visit www.invoquest.us. To speak with a specialist, call us at (888) 392-8990 or reach out through our contact page.
Conclusion
The move toward patient-centric billing is not just a trend—it’s a necessity for modern healthcare providers. By prioritizing transparency and patient satisfaction, providers can create a more efficient billing process that benefits both the practice and its patients. Embracing technology, clear communication, and flexible payment options are key to transforming the billing experience and building lasting trust with patients.